
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Drug/Regimen
- Long-Term Glycaemic Durability of Early Combination Therapy Strategy versus Metformin Monotherapy in Korean Patients with Newly Diagnosed Type 2 Diabetes Mellitus
- Soon-Jib Yoo, Sang-Ah Chang, Tae Seo Sohn, Hyuk-Sang Kwon, Jong Min Lee, Sungdae Moon, Pieter Proot, Päivi M Paldánius, Kun Ho Yoon
- Diabetes Metab J. 2021;45(6):954-959. Published online November 12, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0173
- 55,057 View
- 367 Download
- 3 Web of Science
- 2 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 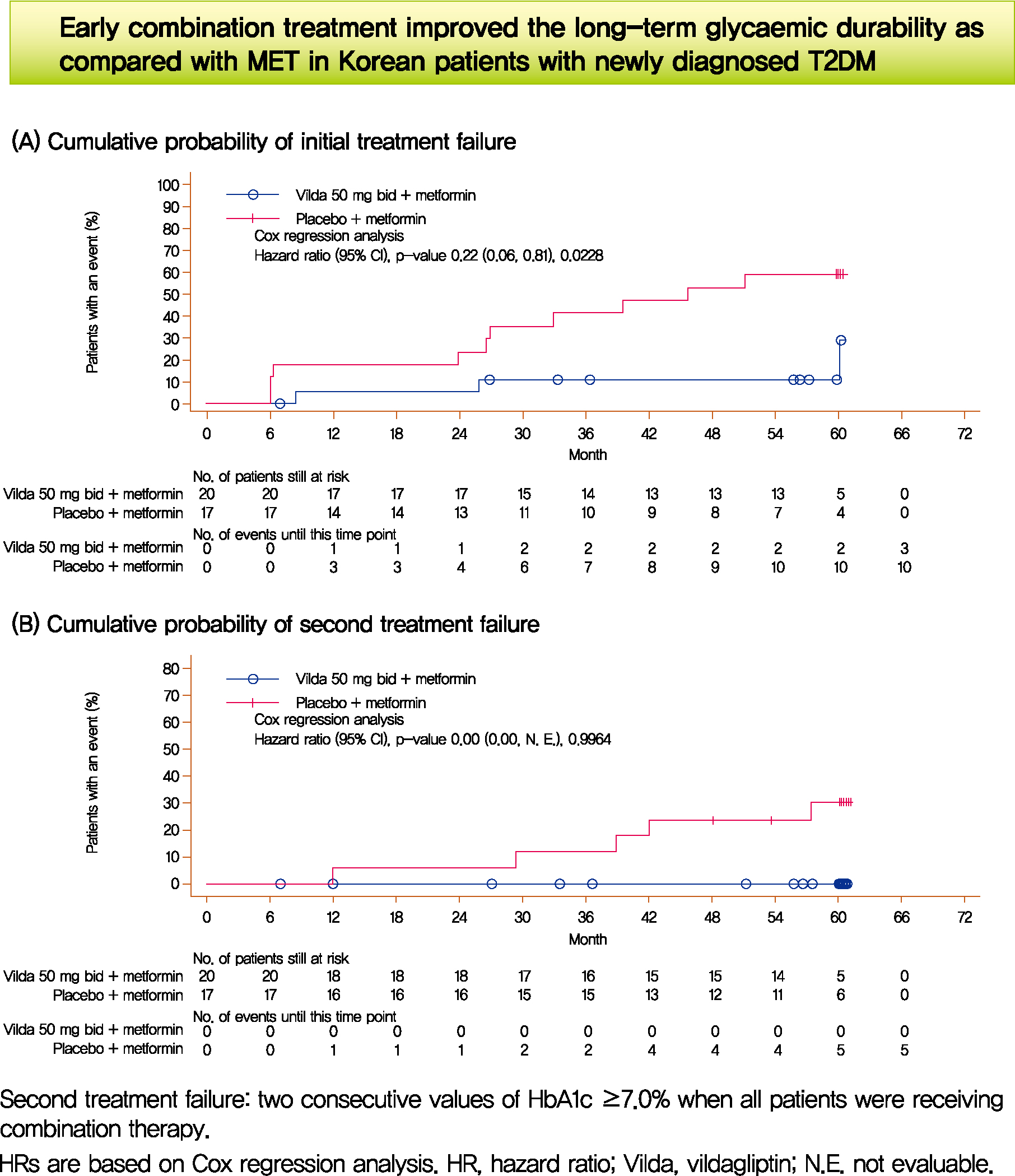
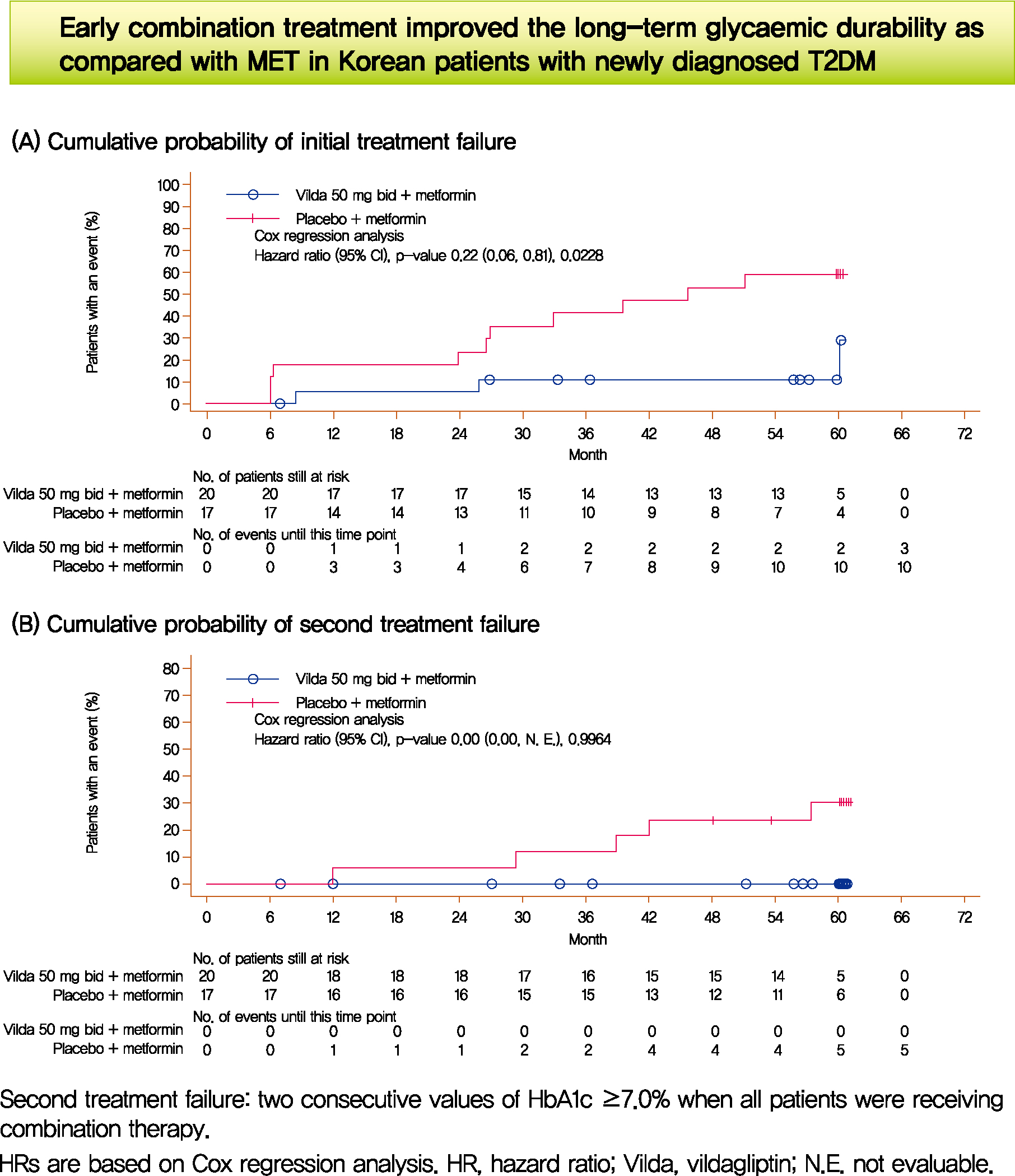
- We assessed the glycaemic durability with early combination (EC; vildagliptin+metformin [MET], n=22) versus MET monotherapy (n=17), among newly-diagnosed type 2 diabetes mellitus (T2DM) enrolled (between 2012 and 2014) in the VERIFY study from Korea (n=39). Primary endpoint was time to initial treatment failure (TF) (glycosylated hemoglobin [HbA1c] ≥7.0% at two consecutive scheduled visits after randomization [end of period 1]). Time to second TF was assessed when both groups were receiving and failing on the combination (end of period 2). With EC the risk of initial TF significantly reduced by 78% compared to MET (n=3 [15%] vs. n=10 [58.7%], P=0.0228). No secondary TF occurred in EC group versus five patients (29.4%) in MET. Patients receiving EC treatment achieved consistently lower HbA1c levels. Both treatment approaches were well tolerated with no hypoglycaemic events. In Korean patients with newly diagnosed T2DM, EC treatment significantly and consistently improved the long-term glycaemic durability as compared with MET.
-
Citations
Citations to this article as recorded by- 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae J
Diabetes & Metabolism Journal.2023; 47(5): 575. CrossRef - 2021 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Kyu Yeon Hur, Min Kyong Moon, Jong Suk Park, Soo-Kyung Kim, Seung-Hwan Lee, Jae-Seung Yun, Jong Ha Baek, Junghyun Noh, Byung-Wan Lee, Tae Jung Oh, Suk Chon, Ye Seul Yang, Jang Won Son, Jong Han Choi, Kee Ho Song, Nam Hoon Kim, Sang Yong Kim, Jin Wha Kim,
Diabetes & Metabolism Journal.2021; 45(4): 461. CrossRef
- 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
- Obesity and Metabolic Syndrome
-
- PF-04620110, a Potent Antidiabetic Agent, Suppresses Fatty Acid-Induced NLRP3 Inflammasome Activation in Macrophages
- Seung Il Jo, Jung Hwan Bae, Seong Jin Kim, Jong Min Lee, Ji Hun Jeong, Jong-Seok Moon
- Diabetes Metab J. 2019;43(5):683-699. Published online October 24, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0112
- 5,415 View
- 66 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Chronic inflammation has been linked to insulin resistance and type 2 diabetes mellitus (T2DM). High-fat diet (HFD)-derived fatty acid is associated with the activation of chronic inflammation in T2DM. PF-04620110, which is currently in phase 1 clinical trials as a selective acyl-CoA:diacylglycerol acyltransferase-1 (DGAT1) inhibitor, is a potent anti-diabetic agent that may be important for the regulation of chronic inflammation in T2DM. However, the mechanisms by which PF-04620110 regulates fatty acid-induced chronic inflammation remain unclear.
Methods PF-04620110 was used
in vitro andin vivo . DGAT1-targeting gRNAs were used for deletion of mouse DGAT1 via CRISPR ribonucleoprotein (RNP) system. The activation of NLRP3 inflammasome was measured by immunoblot or cytokine analysisin vitro andin vivo .Results Here we show that PF-04620110 suppressed fatty acid-induced nucleotide-binding domain, leucine-rich-repeat-containing receptor (NLR), pyrin-domain-containing 3 (NLRP3) inflammasome activation in macrophages. In contrast, PF-04620110 did not change the activation of the NLR family, CARD-domain-containing 4 (NLRC4), or the absent in melanoma 2 (AIM2) inflammasomes. Moreover, PF-04620110 inhibited K+ efflux and the NLRP3 inflammasome complex formation, which are required for NLRP3 inflammasome activation. PF-04620110 reduced the production of interleukin 1β (IL-1β) and IL-18 and blood glucose levels in the plasma of mice fed HFD. Furthermore, genetic inhibition of DGAT1 suppressed fatty acid-induced NLRP3 inflammasome activation.
Conclusion Our results suggest that PF-04620110 suppresses fatty acid-induced NLRP3 inflammasome activation.
-
Citations
Citations to this article as recorded by- Drug Targeting of Acyltransferases in the Triacylglyceride and 1-O-AcylCeramide Biosynthetic Pathways
Maria Hernandez-Corbacho, Daniel Canals
Molecular Pharmacology.2024; 105(3): 166. CrossRef - Possible therapeutic targets for NLRP3 inflammasome-induced breast cancer
Xixi Wang, Junyi Lin, Zhe Wang, Zhi Li, Minghua Wang
Discover Oncology.2023;[Epub] CrossRef
- Drug Targeting of Acyltransferases in the Triacylglyceride and 1-O-AcylCeramide Biosynthetic Pathways
- The Classification of Diabetic Patients Presenting Diabetic Ketoacidosis: The Characteristics of Fulminant Type 1 Diabetes.
- Eun Hee Jang, Jeong Eun Yi, Seung Jae Lee, Sang Hoon Chun, Ki Hyun Baek, Ki Ho Song, Soon Jib Yoo, Jong Min Lee, Kun Ho Yoon, Moo Il Kang, Kwang Woo Lee, Mee Kyung Kim
- Korean Diabetes J. 2008;32(5):428-434. Published online October 1, 2008
- DOI: https://doi.org/10.4093/kdj.2008.32.5.428
- 2,688 View
- 43 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The aim of the study was to classify newly diagnosed diabetic patients who initially presented with diabetic ketoacidosis (DKA) into specific types of diabetes and to describe the clinical and biochemical characteristics of patients with fulminant type 1 DM in Korea. METHODS: Using data from 4 hospitals of CMC from 1 January 1999 to 1 March 2008, we identified all patients who manifested DKA when they were first diagnosed as diabetes. Clinical and laboratory data were reviewed from medical records. RESULTS: We identified 51 newly diagnosed diabetic patients manifested DKA. Among them, 14 (27.4%) patients were classified as autoimmune type 1 DM, 8 (15.7%) as antibody negative type 1 DM, 5 (9.8%) as fulminant type 1, 16 (31.4%) as type 2 DM and 8 (15.7%) as secondary DM. Five patients who fulfilled the criteria of fulminant type 1 DM were older (32.2 +/- 10.7 vs. 15.7 +/- 4.4 years, P = 0.010), had shorter duration of symptoms (4.2 +/- 2.7 vs.16.7 +/- 15.2 days, P = 0.014) and lower stimulated C-peptide levels (0.1 +/- 0.0 vs. 0.7 +/- 0.6 ng/mL, P = 0.050) compared with patients with autoimmune type 1 DM. CONCLUSION Newly diagnosed diabetic patients presenting with DKA composed of heterogenous types of diabetes. The prevalence of fulminant type 1 diabetes among them was 9.8% and the clinical and biochemical characteristics of these patients were different from those of autoimmune type 1 DM. -
Citations
Citations to this article as recorded by- A Case of Severe Diabetic Ketoacidosis in a Child with Type 2 Diabetes
Jaesung Yu, Hyunju Jin, Joontae Ko, Hoseok Kang
Journal of Korean Society of Pediatric Endocrinology.2011; 16(1): 46. CrossRef - A Case of Fulminant Type 1 Diabetes Mellitus Complicated with Ischemic Ileitis
Se-Won Oh, Ju-Ri Park, Yun-Jeong Lee, Hee-Yeong Kim, Ji-A Seo, Nan-Hee Kim, Kyung-Mook Choi, Sei-Hyun Baik, Dong-Seop Choi, Sin-Gon Kim
Journal of Korean Endocrine Society.2009; 24(2): 116. CrossRef
- A Case of Severe Diabetic Ketoacidosis in a Child with Type 2 Diabetes
- A Case of Chronic Inflammatory Demyelinating Polyneuropathy in a Girl with Type 1 DM .
- Yi Sun Jang, Hye Soo Kim, Jong Min Lee
- Korean Diabetes J. 2006;30(2):130-135. Published online March 1, 2006
- DOI: https://doi.org/10.4093/jkda.2006.30.2.130
- 1,665 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - Chronic inflammatory demyelinating polyneuropathy (CIDP) is an immune-mediated disorder characterized by the symmetrical weakness in both proximal and distal muscles for at least 2 months, hyporeflexia or areflexia, nerve conduction abnormalities, and high CSF protein level. Diabetes mellitus, monoclonal gammopathy, hepatitis C infection, HIV infection, SLE, Sjogren syndrome and lymphoma have been associated with CIDP. The incidence of CIDP in diabetes is not known exactly, but occur more common among diabetic than nondiabetic patients. There is sometimes a difficulty in distinguishing between diabetic polyneuropathy and CIDP, but differential diagnosis is important because CIDP is treatable with immune-modulating therapy. We report a case of CIDP in 22-year-old girl with type 1 DM who presented with generalized motor weakness and walking disturbance which were treated with iv immunoglobulin
- Selective beta-Cell Loss and alpha-Cell Expansion in Islets of Type 2 Diabetic Patients.
- Jae Hyoung Cho, In Kyu Lee, Kun Ho Yoon, Seung Hyun Ko, Sun Hee Suh, Jung Min Lee, Sung Rae Kim, Yoo Bae Ahn, Jong Min Lee, Hyun Shik Son, Moo Il Kang, Bong Yun Cha, Kwang Woo Lee, Ho Young Son, Sung Koo Kang
- Korean Diabetes J. 2001;25(2):164-177. Published online April 1, 2001
- 1,287 View
- 26 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
It has been reported that a decrease in the beta-cell mass, may play a major role in the development of type 2 diabetes. Some stimuli that cause beta-cell loss can stimulate neogenesis from precursors as well as replication of matured beta-cells. In an animal-based studies reported that alpha-cells can also be produced in the course of alpha-cell neogenesis, after being treated with streptozotocin. Through this research, we attempted to determine the change of beta-cell mass according to the changes in alpha-cell mass and to characterize the size of the beta-cell nucleus observed in type 2 diabetes. METHOD: To estimate the relative fraction of alpha- and beta-cell mass in the pancreas, we counted beta-cells and alpha-cells by point count method. We also performed a double immunohistochemical staining with glucagon and insulin antibodies to calculate the ratio between these two cells area in the pancreas (A/B ratio). In order to measure the size of the beta-cell nucleus, an immunofluorescence staining of the nucleus and insulin was carried out. Data were gathered from type 2 diabetic subjects (n=19) and normal controls (n=8). RESULTS: Although there was no statistical difference, we observed the tendency of decrease of beta-cell mass and increase of alpha-cell mass in the pancreas of type 2 diabetic patients. The ratio of alpha-to beta-cell area in islet (A/B ratio) increased to 0.81+/-0.76 in diabetic patients compared to control with 0.26+/-0.25 (p<0.01). The mean of the A/B ratios of the islets more than 22,000 micro m2 was 1.64+/-1.10, whereas that of the islets less than 22,000 micro m2 was 0.73+/-0.67 in type 2 diabetic patients (p<0.01). The size of the beta-cell nucleus in both diabetic subjects and normal controls was bigger than that of exocrine cells (p<0.05) and 2.9% of beta-cells in type 2 diabetic subjects showed substantially enlarged nuclei more than M+5SD (M and SD means the average and standard deviation of nucleus size of exocrine cells, respectively) whereas this type of nucleus was found in only 0.5% of beta-cells in normal controls (p<0.05). CONCLUSION: The islet pathology in type 2 diabetes could be characterized by an expansion of alpha-cells associated with the selective loss of beta-cells. Some beta-cells found in diabetes showed a significant increase in size of the nucleus. Through the results from this study, we postulate that enlarged beta-cell nucleus and reverse of A/B ratio in the islets could be a marker of early senescence of beta-cells in patients with type 2 diabetes mellitus.
- Effects of Cilostazol on Insulin Resistance in OLETF Rats.
- Sung Rae Kim, Ki Hyun Baek, Seung Hyun Ko, Jung Min Lee, Sang Ah Chang, Yoo Bae Ahn, Soon Jib Yoo, Jong Min Lee, Hyun Shik Son, Kun Ho Yoon, Moo Il Kang, Bong Yun Cha, Kwang Woo Lee, Ho Young Son, Sung Koo Kang
- Korean Diabetes J. 2001;25(1):63-70. Published online February 1, 2001
- 1,219 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Insulin resistance is one of the major pathophysiology of type 2 diabetes mellitus. It is reported that cilostazol and cyclic AMP phosphodiesterase inhibitor has the anti-platelet effect as well as an improvement of hypertriglyceridemia in addition to vasodilatation. Furthermore, the previous reports indicated that there is a positive relationship between insulin resistance and dyslipidemia. Thus, we investigated the effects of cilostazol on insulin resistance in OLETF rats using the euglycemic hyperinsulinemic glucose clamp technique, and lipid levels. METHODS: Fifteen five months old OLETF rats were fed for 4 weeks(8 treated with cilostazol and 7 were control), and compare to 20 same aged LETO rats (8 treated with cilostazol and 12 were control) through the glucose infusion rate on euglycemic hyperinsulinemic glucose clamp and lipid profiles. RESULTS: The glucose infusion rate was higher in the cilostazol treated OLETF rats than in the non-cilostazol treated OLETF rats (0.021+/-0.0031 vs 0.027+/-0.0036 mL/min). The levels of free fatty acids (2424.8+/-652.7 vs 1061.8+/-223.2 Eq/L), total cholesterol (145.7+/-17.9 vs 115.4+/-7.6 mg/dL) and triglyceride (146.5+/-46.6 vs 76.1+/-12.5 mg/dL) of cilostazol treated OLETF rats were significantly lower than those of non-cilostazol treated OLETF rats. CONCLUSION: This study result suggest that cilostazol may improve the insulin resistance through the improvement of dyslipidemia in OLETF rats.
- The Effect of Metformin Monotherapy in Patients with NIDDM.
- Yu Bae Ahn, Sung Dae Moon, Sang Ah Jang, Jong Min Lee, Hyun Shik Son, Kun Ho Yoon, Moo Il Kang, Bong Yun Cha, Kwang Woo Lee, Ho Young Son, Sung Koo Kang
- Korean Diabetes J. 1997;21(2):185-193. Published online January 1, 2001
- 1,088 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
We performed this study to investigate the effect of metformin on glycemia, insulin secretion and body weight in patients with non-insulin-dependent diabetes melltus(NIDDM) who could not aehieve satisfactory glycemic control by sulfonylurea or diet therapy. METHODS: A total of 167 patients with NIDDM were included in this study. At baseline the patients underwent anthropometry and a 75g oral glucose tolerance test. Jn addition, levels of hemoglobin Alc (HbAlc), setum lipids, fasting and postprandial 2hr glucose were measured. Metformin was given in an initial dose of 500mg twice daily and increased by 500mg every month as long as the fasting blood sugar(FBS) concentration exceeded 7.8mmol/L and the side effects were tolerable. After 3 rnonths of metformin therapy we defined a responder as a patient who experienced a FBS of under 7.8 mmol/L or a HbAlc of under 7%. Patients who failed to respond to metformin monotherapy were excluded in the study. Anthrapometric changes and results of a 75 g oral glucose tolerance test were reevaluated in the responder group after 6 months of metformin treatment. RESULTS: I) The overall response rate to metformin mono-therapy was 55.6%(79/142) in the study population. 2) There were significant changes in body weight (64.4+/-8.2 vs 62.9+/-8.4 kg, p(0.01) and body mass index(25.3+/-2.3 vs 24.6+/-2.3kg/m, p<0.01) during metformin treatment. 3) There were significant decreases in the fasting, postprandial 2hr serum glucose(10.1+/-2.8 vs 7.9+1.6, 15,2+/-5.0 vs 12.2+/-3.9 mmol/L, p 0.01) and HbAlc levels(8.4+/-1.7 vs 6.5+/-0.9%, p<0.05) after 6 months of metformin treatment. 4) There were significant decreases in the levels of AUC[g](59.2+/-15.5 vs 49.4+/-9.4mmol L-1. Min-1, p =C0.01) without changes of AUC[I] and AUC[I]/ AUC[g] ratio (558.0+486.0 vs 536.4+374.4 pmol.L-1. Min-1, p=0.71, 11.7+/-13.0 vs 11.8+/-10.0, p=0.89). 5) The incidence of side effects was 25% in the study population, but most of them were mild and fade away with continuous use of metformin, CONCLUSION: Metforrnin monotherapy improved glycemic control in NlDDM patients who failed to respond to diet or sulfonylurea therapy and may be a useful hypoglycemic agent for the treatment of NIBDM.
- Case reports on diabetes mellitus caused by malnutrition-related diabetes mellitus and chronic relapsing pancreatitis.
- Yong Joo Kim, Jong Min Lee, Hyun Shik Son, Bong Yun Cha, Kwang Woo Lee, Ho Young Son, Sung Ku Kang, Young Taek Song, Sang In Shim
- Korean Diabetes J. 1992;16(4):341-346. Published online January 1, 2001
- 866 View
- 18 Download
- 3 cases of emphysematous pyelonephritis complicated in diabetics.
- Jong Min Lee, Seung Ho Bang, Chae Ho Han, Hyun Shik Son, Kun Ho Yoon, Sung Ku Kang, Bong Yun Cha, Kwang Woo Lee, Ho Young Son
- Korean Diabetes J. 1992;16(4):335-340. Published online January 1, 2001
- 912 View
- 16 Download
- Prevalence of micro and macroalbuminuria in relation to hypertension and chronic diabetic vascular complications among type II diabeticpatients.
- Hyuk Ho Kwon, Je Ho Han, Jong Min Lee, Soon Jip Yoo, Hyun Sik Son, Kun Ho Yoon, Moo Il Kang, Jwan Soo Hong, Bong Yun Cha, Kwang Woo Lee, Ho Young Son, Sung Ku Kang
- Korean Diabetes J. 1992;16(4):317-324. Published online January 1, 2001
- 941 View
- 16 Download

 KDA
KDA
 First
First Prev
Prev





